How to Treat Achalasia?
- November 10, 2023
- No Comments
What is Achalasia?
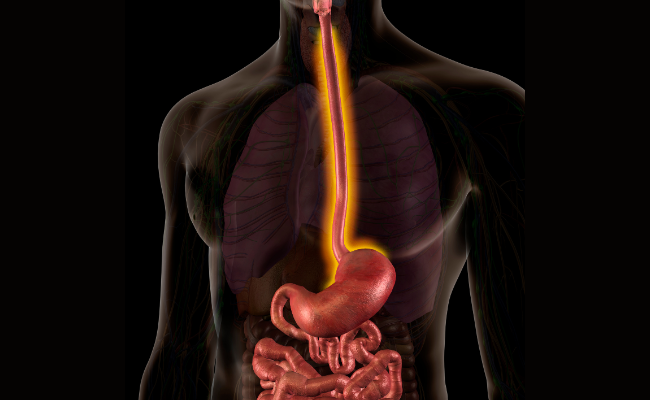
Achalasia is a rare yet significant disorder impacting the esophagus, the muscular tube linking the throat to the stomach. This condition disrupts the standard functioning of the lower esophageal sphincter (LES), a muscular ring located at the esophagus-stomach junction. The LES ordinarily relaxes during swallowing, facilitating the passage of food from the esophagus to the stomach. However, individuals with achalasia experience improper relaxation of the LES, resulting in a spectrum of symptoms and potential complications. This disorder manifests as an inability of the esophagus to propel food and liquids effectively into the stomach, where the LES, a crucial muscular ring, fails to relax as needed for smooth digestion.
Why Does Achalasia Occur?
The exact cause of achalasia remains somewhat elusive, but it is believed to be associated with the degeneration of nerve cells in the esophagus. These nerve cells, responsible for coordinating muscle contractions, deteriorate over time, leading to dysfunction in the LES. Additionally, autoimmune factors and a genetic predisposition may contribute to the development of achalasia. The result is a condition where the normal peristaltic movements of the esophagus are compromised, causing difficulty in the passage of food into the stomach.
How is Achalasia Diagnosed?
Diagnosing achalasia involves a thorough examination that includes a medical history assessment, a physical examination, and various diagnostic tests to confirm the presence of the condition.
- Esophageal Manometry: This diagnostic test measures the pressure in the esophagus and assesses the function of the LES. It provides insights into whether the LES is relaxing appropriately during swallowing, aiding in the confirmation of achalasia.
- Barium Swallow Test: During this test, the patient swallows a liquid containing barium, which makes the esophagus visible on X-rays. Barium swallow imaging can reveal the narrowing of the esophagus and the pooling of barium due to impaired emptying, indicative of achalasia.
- Endoscopy: A thin, flexible tube with a camera, known as an endoscope, is passed through the mouth and into the esophagus. This procedure allows for visual inspection of the LES and the esophagus, helping rule out other potential causes of symptoms and confirming the diagnosis of achalasia.
Treatment Solutions for Achalasia:
- Dilation (Balloon Therapy): Dilation, a non-surgical procedure, involves the inflation of a balloon at the narrowed LES to stretch and widen it. This helps improve the passage of food from the esophagus into the stomach. While effective, repeat dilations may be necessary over time to maintain the desired outcome.
- Botulinum Toxin (Botox) Injections: In some cases, botulinum toxin injections may be administered directly into the LES during an endoscopy. This temporarily paralyzes the muscle, allowing for easier food passage. However, it's important to note that the effects are temporary, and individuals may require repeated injections.
- Surgery (Myotomy): Surgical intervention, known as myotomy, involves cutting or dissecting the LES to allow for better relaxation and improved food passage. This procedure can be conducted through traditional open surgery or through minimally invasive techniques such as laparoscopy.
- Peroral Endoscopic Myotomy (POEM): A relatively newer and less invasive procedure, POEM utilizes an endoscope to create a tunnel in the esophagus. This allows for myotomy without external incisions, resulting in a quicker recovery time compared to traditional surgery.
Benefit Points of Achalasia Treatment:
- Improved Swallowing Function: The primary objective of achalasia treatment is to enhance swallowing function. By addressing the underlying cause and improving the relaxation of the LES, individuals experience improved ease of swallowing.
- Relief from Symptoms: Treatment options, whether dilation, botulinum toxin injections, or surgical interventions, provide relief from troublesome symptoms associated with achalasia. This includes regurgitation, chest pain, and weight loss, contributing to an overall improvement in quality of life.
- Prevention of Complications: Timely intervention and treatment help prevent potential complications associated with achalasia, such as the development of esophageal strictures or aspiration pneumonia. Proactive management reduces the risk of long-term complications.
- Options for Individualized Care: The diverse range of treatment options allows for individualized care based on the severity of symptoms, patient preferences, and the expertise of the healthcare provider. This personalized approach ensures that each patient receives tailored and effective treatment.
- Long-Term Management: While some treatments may require periodic repetition, successful interventions offer long-term management of achalasia. This enables individuals to lead a more comfortable and functional life, not constantly burdened by the symptoms of the condition.
- Less Invasive Techniques: Minimally invasive procedures like POEM offer the benefits of effective treatment with reduced invasiveness. These techniques often result in shorter recovery times and potentially fewer complications compared to traditional surgical approaches.
- Comprehensive Evaluation and Diagnosis: The diagnostic methods employed for achalasia provide a comprehensive evaluation, ensuring an accurate diagnosis and differentiation from other esophageal disorders. This precision is crucial for determining the most suitable and effective treatment approach.
Comments (0)