How to Treat Nodular Nonsuppurative Panniculitis?
- December 11, 2023
- No Comments
What is Nodular Nonsuppurative Panniculitis?
Nodular nonsuppurative panniculitis (NNP) is a rare inflammatory condition impacting the subcutaneous fat tissue, resulting in the development of tender nodules primarily on the lower extremities, buttocks, and thighs. The intricacy of NNP arises from a multitude of contributing factors, making its comprehension and management a complex task. The challenge lies in the diverse manifestations of the disorder and the crucial need for a personalized treatment approach. In this exploration, we aim to unravel the intricacies of NNP by examining its origins, manifestations, and diverse treatment strategies, all aimed at achieving optimal outcomes for affected individuals.
Why Does Nodular Nonsuppurative Panniculitis Occur?
While the exact cause of NNP remains elusive, several factors have been identified as potential contributors to its development. Autoimmune diseases, including lupus erythematosus and rheumatoid arthritis, are associated with an increased risk of NNP. Infections caused by bacteria or fungi have also been implicated, acting as triggers that set off an inflammatory response leading to the formation of nodules. Furthermore, certain medications, such as oral contraceptives and corticosteroids, have been linked to the onset of NNP, highlighting the intricate interplay between immune dysregulation and external factors.
How Does Nodular Nonsuppurative Panniculitis Manifest?
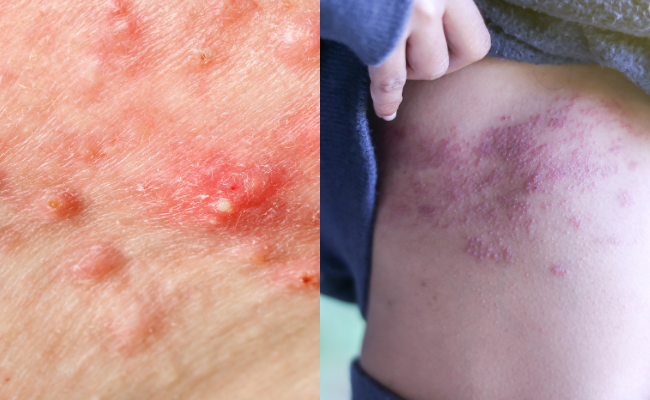
The clinical presentation of NNP is marked by the abrupt onset of painful subcutaneous nodules. These nodules, accompanied by redness and warmth at the affected site, create a characteristic pattern on the skin. The lower extremities, buttocks, and thighs are the primary sites of involvement. In more severe cases, the nodules may progress to ulceration or skin necrosis, necessitating immediate attention and intervention. Diagnosing NNP requires a meticulous clinical evaluation, incorporating a detailed medical history, thorough physical examination, and often a skin biopsy for definitive confirmation.
Navigating Treatment Strategies: A Multifaceted Approach
The management of Nodular Nonsuppurative Panniculitis is complex, emphasizing the need to address underlying causes, relieve symptoms, and prevent potential complications. Several treatment strategies are commonly employed in clinical practice:
- Corticosteroids: Systemic corticosteroids, such as prednisone, constitute a mainstay in the treatment of NNP. Initial high doses may be required to control inflammation, followed by a gradual tapering to a maintenance level to prevent relapse.
- Immunosuppressive Medications: In cases where autoimmune diseases are implicated, immunosuppressive medications like methotrexate or azathioprine are often prescribed. These agents work to modulate the immune response, mitigating further inflammatory processes.
- Antibiotics or Antifungals: If an infectious etiology is identified, targeted antimicrobial therapy becomes paramount. Appropriate antibiotics or antifungals are employed to eliminate the underlying infection triggering NNP.
- Pain Management: Analgesics, particularly nonsteroidal anti-inflammatory drugs (NSAIDs), play a crucial role in managing the pain and discomfort associated with NNP. This aspect of treatment is essential for improving the overall quality of life for affected individuals.
- Supportive Therapies: Beyond specific pharmacological interventions, supportive measures such as the application of cold compresses and elevation of affected limbs contribute to symptomatic relief. These measures aim to reduce swelling and facilitate the healing process.
Realizing the Benefits: Navigating Towards Improved Quality of Life
Effective management of NNP translates into several tangible benefits for individuals grappling with this condition:
- Pain Relief: Treatment significantly alleviates the pain and tenderness associated with NNP, fostering a considerable improvement in the overall quality of life for affected individuals.
- Complication Prevention: Timely intervention reduces the risk of complications, including ulceration, skin necrosis, and secondary infections, safeguarding the well-being of patients.
- Disease Control in Autoimmune Cases: Managing the underlying autoimmune condition not only addresses the current episode of NNP but also contributes to preventing recurrence and minimizing the risk of systemic complications associated with autoimmune diseases.
- Improved Quality of Life: Addressing the root cause and effectively managing symptoms lead to an overall enhancement of the well-being of individuals navigating life with nodular nonsuppurative panniculitis.
- Recurrence Prevention: By adopting a holistic approach that treats the underlying cause and provides ongoing care, the likelihood of recurrence is diminished. This empowers individuals to better manage and control the condition over the long term.
Comments (0)