How Video Assisted Thoracoscopic Surgery (VATS) Works?
- December 12, 2023
- No Comments
What is Video Assisted Thoracoscopic Surgery (VATS)?
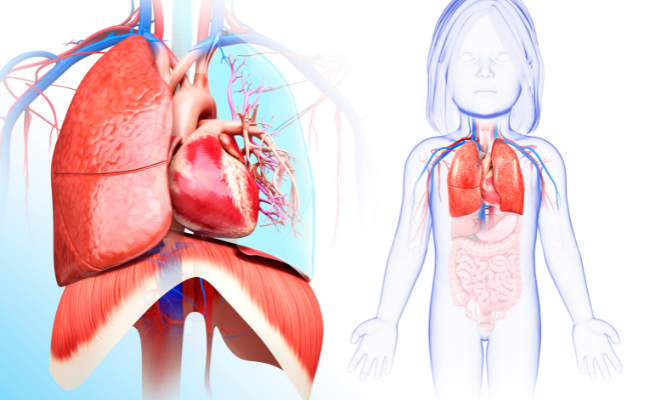
Video-assisted thoracic surgery (VATS) is a minimally invasive procedure designed to diagnose and treat specific conditions affecting the chest area. This innovative surgical approach involves the insertion of a thin tube equipped with a tiny video camera, known as a thoracoscope, into a small incision in the chest. The thoracoscope provides a visual feed, allowing healthcare providers to observe the interior of the chest cavity. Simultaneously, surgical instruments are introduced through separate small incisions, guided by the images from the thoracoscope, facilitating precise and effective procedures. This technique is also referred to as video-assisted thoracoscopy.
Why Video Assisted Thoracoscopic Surgery?
The traditional approach to thoracic surgeries, involving large incisions, often resulted in considerable postoperative pain, extended recovery periods, and an increased risk of complications. VATS was developed as a response to these challenges, aiming to reduce the trauma associated with surgery and enhance patient outcomes. The primary motivations behind the adoption of VATS include a desire to minimize scarring, accelerate postoperative recovery, and decrease the overall impact of the surgical procedure on the patient's well-being.
How is Video Assisted Thoracoscopic Surgery Performed?
The VATS procedure involves several key steps, each contributing to the overall success of the surgery and the well-being of the patient:
- Patient Preparation: Before initiating the VATS procedure, patients undergo a comprehensive evaluation, which may include imaging studies to assess the condition of the thoracic region. General anesthesia is administered to ensure the patient is completely unconscious and pain-free during the surgery.
- Incision Placement: One of the distinguishing features of VATS is the use of small incisions, typically ranging from 0.5 to 1.5 centimeters in size. These incisions serve as ports for the insertion of the thoracoscope (a thin tube with a camera and light) and other specialized instruments.
- Thoracoscopy: The thoracoscope is inserted through one of the small incisions, providing the surgeon with a magnified and illuminated view of the internal structures of the chest cavity. The real-time visuals are displayed on a monitor, allowing the surgical team to navigate and execute the procedure with precision.
- Instrument Insertion: Additional small incisions are made to accommodate specialized instruments used for manipulating tissues, cutting, and suturing. These instruments are designed to replicate the movements of the surgeon's hands, offering precise control and maneuverability.
- Procedure Execution: Guided by the visuals from the thoracoscope, the surgeon performs the necessary steps of the procedure. Common VATS procedures include lung biopsies, lobectomies, pleural effusion drainage, and sympathectomies, among others.
- Closure: Once the surgical steps are completed, the instruments are removed, and the small incisions are closed with sutures or staples. Unlike traditional surgeries that may require a chest tube for postoperative drainage, VATS often involves less drainage due to its minimally invasive nature.
Treatment Solutions with VATS:
- Lung Biopsies: VATS is frequently employed for lung biopsies, enabling the removal of tissue samples for diagnostic purposes. This is particularly valuable in cases where the identification and diagnosis of lung cancer or other pulmonary conditions are crucial for determining the appropriate course of treatment.
- Lobectomy: In situations where a portion of the lung needs to be removed, as in cases of lung cancer or certain lung diseases, VATS allows for the precise removal of the affected lobe. This targeted approach minimizes damage to healthy surrounding tissue and facilitates a more efficient recovery.
- Pleural Effusion Drainage: VATS is an effective method for draining fluid accumulation in the pleural space, a condition known as pleural effusion. By providing a less invasive means of addressing this issue, VATS helps alleviate symptoms such as chest pain and difficulty breathing.
- Sympathectomy: For conditions like hyperhidrosis, characterized by excessive sweating, VATS can be utilized to perform a sympathectomy. This involves interrupting the sympathetic nerve signals responsible for the excessive sweating, offering patients relief from this often debilitating condition.
Benefits of Video Assisted Thoracoscopic Surgery:
- Minimized Scarring: One of the most apparent benefits of VATS is the minimized scarring associated with the smaller incisions. Patients undergoing VATS often express satisfaction with the cosmetic outcome, as the scars are less prominent and visible compared to those resulting from traditional open surgeries.
- Reduced Pain and Discomfort: The smaller incisions and reduced trauma to surrounding tissues in VATS contribute to decreased postoperative pain and discomfort. This is a significant advantage for patients, as it not only enhances their overall experience but also facilitates a quicker recovery.
- Quicker Recovery Time: The minimally invasive nature of VATS translates to a quicker recovery for patients. They typically experience a faster return to their daily activities, including work and exercise, compared to individuals undergoing traditional open surgery. This accelerated recovery is particularly beneficial for patients seeking a swift return to normalcy.
- Lower Risk of Complications: VATS is associated with a lower risk of complications, including infection, bleeding, and respiratory issues. The reduced trauma to tissues and organs during the procedure contributes to a generally smoother recovery process, minimizing the likelihood of adverse events.
- Improved Visualization: The use of a thoracoscope in VATS provides surgeons with a magnified and illuminated view of the surgical site. This enhanced visualization allows for greater precision and accuracy during procedures, ultimately improving overall outcomes. Surgeons can navigate complex anatomical structures more effectively, reducing the risk of errors.
- Less Impact on Respiratory Function: Unlike open surgeries that may involve spreading the ribs, VATS minimizes the impact on respiratory function. This is particularly advantageous for patients with compromised lung function, as it helps preserve their respiratory capacity during and after the surgical intervention.






Comments (0)
No comments yet