How to Treat Thrombotic Thrombocytopenic Purpura Haemolytic Uraemic Syndrome?
- September 27, 2023
- No Comments
What is Thrombotic Thrombocytopenic Purpura Haemolytic Uraemic Syndrome (TTP-HUS)?
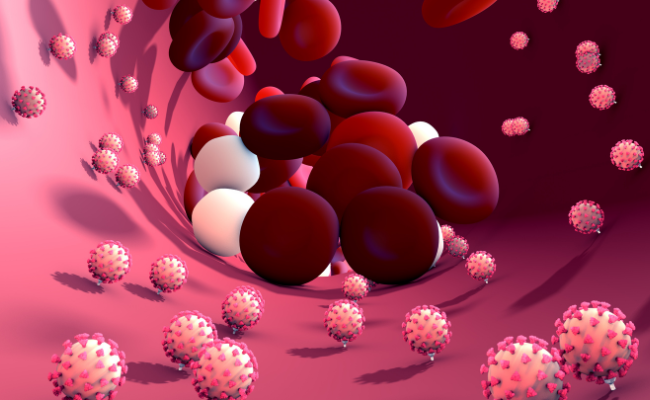
Thrombotic Thrombocytopenic Purpura Haemolytic Uraemic Syndrome (TTP-HUS), often referred to as TTP, HUS, or TTP-HUS, is a rare and potentially life-threatening medical condition that impacts blood and blood vessels. It is characterized by the formation of blood clots within small vessels throughout the body, causing a decrease in platelet count and damage to red blood cells. This can lead to severe complications affecting various organs, including the kidneys, brain, and heart. These conditions share similarities, including low platelet counts, microangiopathic hemolytic anemia, and ischemic symptoms, all resulting from platelet aggregation in small arteries, leading to tissue damage.
Why is TTP-HUS a Concern?
TTP-HUS is a significant concern due to its potential for severe complications and the rapid onset of symptoms. If left untreated, it can lead to kidney failure, stroke, heart attack, and even death. Understanding how to treat TTP-HUS is crucial in preventing these life-threatening consequences.
How to Treat TTP-HUS?
The treatment of TTP-HUS involves a combination of medical interventions aimed at addressing the underlying causes and managing the associated complications. Here are the key components of TTP-HUS treatment:
Plasma Exchange (Plasmapheresis):
- Plasma exchange is the cornerstone of TTP-HUS treatment. During this procedure, the patient's blood is separated into its components, and the plasma (which contains the abnormal proteins causing clot formation) is removed and replaced with fresh frozen plasma.
- This helps remove the harmful substances from the blood and restore normal blood flow.
Corticosteroids:
- In addition to plasma exchange, corticosteroid medications like prednisone are often prescribed to reduce inflammation and suppress the immune system's response.
- This can help prevent further damage to blood vessels and platelet destruction.
Immunosuppressive Therapy:
- In some cases, immunosuppressive medications such as rituximab may be used to target the immune system's abnormal response that triggers TTP-HUS.
Management of Complications:
- Depending on the severity and extent of organ damage, additional treatments may be necessary.
- This may include dialysis for kidney failure, anticoagulants to prevent blood clots, and medication to control high blood pressure.
Treatment of Underlying Causes:
- In cases where TTP-HUS is secondary to an underlying condition, such as an autoimmune disorder or cancer, treating the root cause is essential for long-term management.
Treatment Solutions
- Early Diagnosis: Rapid diagnosis is crucial for effective treatment of TTP-HUS. Healthcare providers must be vigilant in recognizing the symptoms and conducting the necessary tests to confirm the condition.
- Plasma Exchange Expertise: Plasma exchange requires specialized equipment and expertise. Access to facilities with experienced medical teams trained in performing plasmapheresis is essential for effective treatment.
- Multidisciplinary Approach: TTP-HUS often involves multiple organs, so a team of specialists, including hematologists, nephrologists, and neurologists, may be required to provide comprehensive care.
- Long-Term Monitoring: After initial treatment, patients with TTP-HUS require ongoing monitoring to assess their response to therapy and to detect any potential relapses or complications.
Benefits of Treating TTP-HUS
- Life-saving Intervention: Timely and appropriate treatment of TTP-HUS can be life-saving. Plasma exchange and other therapies can rapidly reverse the dangerous effects of clot formation and organ damage.
- Prevention of Organ Damage: Effective treatment can prevent or minimize organ damage, particularly in the kidneys and brain, which are commonly affected by TTP-HUS.
- Improved Quality of Life: Treating TTP-HUS can improve the patient's overall quality of life by preventing long-term complications and reducing the risk of relapses.
- Preventing Recurrence: Identifying and treating any underlying conditions or triggers can help prevent the recurrence of TTP-HUS.
Comments (0)