What to do incase of Thyroid Cancer?
- January 04, 2024
- No Comments
What is Thyroid Cancer?
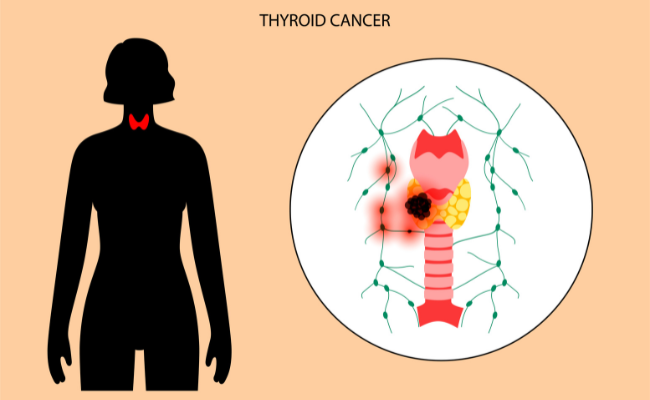
Thyroid cancer is a form of endocrine cancer that develops within the thyroid, a small gland resembling a butterfly situated at the base of the neck. Responsible for producing hormones that govern metabolism, the thyroid plays a pivotal role in regulating essential bodily functions such as body temperature, blood pressure, and heart rate. This relatively uncommon but serious cancer type arises when genetic mutations trigger uncontrolled cell growth, resulting in the formation of tumors within the thyroid gland.
Why Does Thyroid Cancer Occur?
The precise cause of thyroid cancer remains elusive, but several risk factors have been identified. Exposure to high levels of radiation, whether through medical treatments or environmental factors, increases the likelihood of developing thyroid cancer. Additionally, individuals with a family history of thyroid cancer or certain genetic conditions, such as familial medullary thyroid cancer, are at an elevated risk. Gender and age also contribute to the risk profile, with females and individuals over the age of 30 being more susceptible.
The thyroid gland is susceptible to cancer due to its role in regulating hormones essential for metabolism. Disruptions in this delicate hormonal balance can create an environment conducive to the development of cancerous cells.
How is Thyroid Cancer Diagnosed?
- The diagnosis of thyroid cancer often begins with a routine physical examination or the observation of symptoms such as a lump or swelling in the neck, difficulty swallowing, or changes in voice. Further diagnostic tests are then employed to confirm the presence of thyroid cancer and determine its type and stage.
- One of the primary diagnostic tools is ultrasound imaging, which allows healthcare professionals to visualize the thyroid gland and identify any abnormalities. Fine needle aspiration (FNA) biopsy is another common procedure where a small sample of tissue is extracted from the thyroid for examination under a microscope. Blood tests may also be conducted to assess thyroid function and identify any hormonal imbalances.
- Once a diagnosis is confirmed, the cancer is categorized based on its type (papillary, follicular, medullary, or anaplastic) and its stage (extent of spread). This information is crucial in devising an appropriate and effective treatment plan.
Treatment Solutions for Thyroid Cancer
The treatment of thyroid cancer is multifaceted, involving various therapeutic modalities tailored to the specific characteristics of the cancer and the overall health of the patient. Common treatment options include:
- Surgery: The cornerstone of thyroid cancer treatment is often surgical intervention. A thyroidectomy, the removal of all or part of the thyroid gland, is the primary surgical procedure. In some cases, nearby lymph nodes may also be removed to prevent the spread of cancer.
- Radioactive Iodine Therapy: Following surgery, patients may undergo radioactive iodine therapy to eliminate any remaining thyroid tissue or cancer cells. Radioactive iodine is administered orally, and its radioactivity specifically targets and destroys thyroid cells.
- Thyroid Hormone Replacement Therapy: Since the thyroid gland is either partially or entirely removed during surgery, patients may need lifelong thyroid hormone replacement therapy. This ensures the maintenance of normal thyroid function, regulating metabolism and preventing the recurrence of cancer.
- External Beam Radiation Therapy: In cases where cancer has spread beyond the thyroid or if the tumor is inoperable, external beam radiation therapy may be employed. This treatment involves directing focused beams of high-energy radiation at the cancerous cells to destroy them.
- Targeted Therapies: Advanced or recurrent cases of thyroid cancer may be treated with targeted therapies. These medications are designed to interfere with specific molecules involved in the growth and spread of cancer cells.
Benefits of Early Detection and Treatment
- Increased Survival Rates: The early detection of thyroid cancer significantly improves the chances of successful treatment and long-term survival. Timely intervention allows for the removal of cancerous cells before they have the opportunity to spread to other parts of the body.
- Minimized Treatment Intensity: Detecting thyroid cancer in its early stages often results in less aggressive treatments. Smaller tumors confined to the thyroid gland may be successfully treated with surgery alone, eliminating the need for more extensive interventions.
- Improved Quality of Life: Timely treatment not only addresses the cancer itself but also helps manage symptoms and prevent the progression of the disease. This contributes to an improved quality of life for individuals diagnosed with thyroid cancer.
- Prevention of Complications: Early detection and treatment reduce the risk of complications associated with thyroid cancer. This includes the prevention of the cancer spreading to other organs or the recurrence of the disease.
- Emotional and Psychological Well-being: The psychological impact of a cancer diagnosis cannot be overstated. Early identification and effective treatment can alleviate anxiety and uncertainty for patients and their families, fostering emotional and psychological well-being.
Comments (0)